Medical billing is a critical yet often overlooked profession within the healthcare industry. Medical billers ensure that healthcare providers receive timely and accurate payments for their services, acting as the financial bridge between doctors, insurance companies, and patients. This article delves into every aspect of the profession, from daily tasks to career pathways, providing an exhaustive understanding of what it means to work as a medical biller.
Understanding the Role of a Medical Biller
A medical biller is responsible for translating healthcare services into financial claims. When a patient receives care—whether it’s a routine check-up, surgery, or diagnostic test—the medical biller ensures the provider is reimbursed by insurance companies, government programs (like Medicare or Medicaid), or the patient. This process involves meticulous attention to detail, knowledge of medical codes, and familiarity with insurance policies.
Daily Responsibilities
The day-to-day work of a medical biller revolves around accuracy and efficiency. They begin by reviewing patient records and verifying insurance coverage. Once a healthcare provider assigns diagnostic and procedural codes (a task often handled by a medical coder), the biller uses these codes to prepare claims. These claims are submitted electronically to insurance companies using specialized software such as Epic, Medisoft, or AdvancedMD.
For example, if a patient undergoes a blood test (coded as CPT 80053), the biller ensures the code matches the insurer’s requirements and that the claim includes all necessary documentation, such as the doctor’s notes. If the claim is denied—a common occurrence due to errors like incorrect patient information or mismatched codes—the biller investigates the issue, corrects the mistake, and resubmits the claim.
Beyond claims, medical billers also generate invoices for patients. This involves explaining complex billing terms like deductibles, copayments, and out-of-pocket maximums in simple language. They may set up payment plans for patients struggling with high medical costs, balancing empathy with the need to recover payments for their employer.
Types of Medical Billers
The field of medical billing is diverse, with roles tailored to specific healthcare settings:
-
Professional Billers
These individuals work in private practices or clinics, handling claims for routine services like doctor visits, lab tests, and vaccinations. Their challenges include managing high patient turnover and staying updated on coding changes for common procedures. -
Institutional Billers
Found in hospitals, institutional billers manage complex claims for inpatient stays, emergency room visits, and surgeries. For instance, billing for a three-day hospital stay involving surgery and post-operative care requires familiarity with DRG (Diagnosis-Related Group) codes, which determine reimbursement rates for inpatient services. -
Dental Billers
Specializing in dental care, these billers use codes unique to procedures like fillings (D2140) or root canals (D3330). They must navigate dental-specific insurance policies, which often have annual maximums and strict pre-authorization rules. -
Behavioral Health Billers
Working in mental health clinics, these professionals bill for therapy sessions, psychiatric evaluations, and addiction treatment. Stigma around mental health can sometimes lead to delayed payments, requiring billers to communicate sensitively with patients and insurers. -
Remote Billers
With the rise of telehealth, many billers now work from home, managing claims for virtual consultations. This role demands proficiency in digital tools like Zoom-integrated EHR systems and adherence to evolving telehealth billing regulations.
Salary and Earning Potential
A medical biller’s salary varies based on experience, location, and certifications.
| Experience Level | Average Salary | Monthly Earnings |
|---|---|---|
| Entry-Level (0–2 yrs) | $35,000–$40,000 | ~$2,900–$3,300 |
| Mid-Career (3–5 yrs) | $45,000–$55,000 | ~$3,750–$4,580 |
| Experienced (5+ yrs) | $55,000–$70,000 | ~$4,580–$5,830 |
Additional Earnings
Many employers offer bonuses for reducing claim denial rates. A biller who lowers denials by 15% might receive a $2,000 annual bonus. Remote positions sometimes include a 5–10% pay premium due to cost savings on office space.
How to Become a Medical Biller
Education
While a high school diploma is the minimum requirement, most employers prefer candidates with postsecondary training. Certificate programs, such as those offered by Penn Foster or the American Medical Billing Association (AMBA), cover essential topics like medical terminology, insurance protocols, and EHR software. These programs typically take 6–12 months to complete.
Associate degrees in healthcare administration or medical billing provide a broader foundation, including courses in anatomy, ethics, and healthcare law. These two-year programs are ideal for those seeking leadership roles.
| Certification | Issuing Body | Cost | Exam Focus |
|---|---|---|---|
| CPB | AAPC | $399 | Insurance guidelines, coding |
| CMRS | AMBA | $299 | Reimbursement strategies |
| CBCS | NHA | $155 | Billing basics, compliance |
Gaining Experience
Internships at local clinics or hospitals provide hands-on training. For example, an intern might shadow a senior biller to learn how to process Medicare claims or resolve denied invoices. Apprenticeships, often partnered with organizations like AHIMA, combine paid work with mentorship.
A Day in the Life of a Medical Biller
A typical day starts with reviewing denied claims from the previous day. Suppose a claim for a patient’s MRI was denied due to an incorrect ICD-10 code. The biller cross-references the doctor’s notes, corrects the code (e.g., changing M54.5 to M54.6 for lumbar pain), and resubmits the claim.
By mid-morning, the biller shifts to patient invoicing. They might call a patient to explain a $1,200 bill for a broken arm treatment, breaking down costs like the X-ray ($150), cast application ($300), and physician fee ($750).
In the afternoon, the focus turns to compliance. The biller audits recent claims to ensure adherence to HIPAA privacy rules and Medicare guidelines. They might attend a webinar on 2024 CMS updates to stay current.
Challenges in Medical Billing
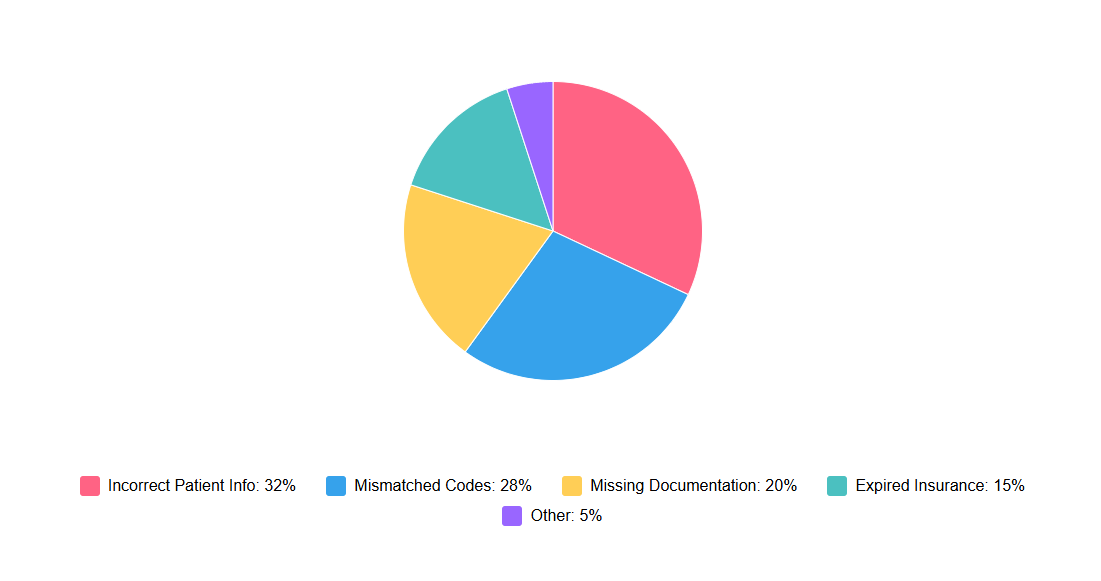
Claim Denials
Approximately 10–20% of claims are initially denied. Common reasons include typos in patient IDs, expired insurance, or mismatched codes. For example, billing CPT 99213 (a mid-level office visit) without supporting documentation of a 15-minute consultation can trigger a denial.
Common Reasons for Claim Denials
 Claim Denials">
Claim Denials">
Regulatory Changes
Healthcare laws evolve constantly. In 2024, CMS introduced new rules for telehealth billing, requiring modifiers like GT (telehealth service) to be appended to claims. Billers must track these changes through newsletters, workshops, or professional networks.
Patient Communication
Many patients are unaware of how insurance works. A biller might spend 30 minutes explaining why their insurance denied coverage for an MRI, only to face frustration. Empathy and clear communication are vital.
Career Advancement and Future Trends
Career Pathways
Experienced billers can advance to roles like:
-
Billing Supervisor: Manages a team of billers, trains new hires, and oversees claim accuracy.
-
Revenue Cycle Manager: Optimizes the entire billing process for a hospital or clinic, aiming to reduce denials and speed up payments.
Emerging Trends
-
Artificial Intelligence: Tools like Automoss scan claims for errors before submission, reducing denials by 25%.
-
Global Outsourcing: Clinics increasingly outsource billing to countries like India, where labor costs are lower. While this saves money, it raises concerns about data security and quality control.
Ethical Considerations
Medical billers handle sensitive data and must adhere to strict ethical standards. For example, upcoding—billing for a more expensive service than provided—is illegal and can result in fines or imprisonment. A 2023 case in Florida saw a biller fined $10,000 for falsely coding routine exams as "complex" to inflate reimbursements.
Conclusion
Medical billing is a dynamic, detail-oriented career that plays a vital role in healthcare sustainability. By mastering technical skills, staying updated on regulations, and prioritizing patient communication, medical billers ensure the financial health of providers while navigating an ever-changing industry. Whether working in a hospital, dental office, or from home, this profession offers stability, growth, and the satisfaction of keeping healthcare accessible.