Precise Billing for Genetic Testing & Counseling Services
From hereditary cancer panels and pharmacogenomics to prenatal screening and metabolic testing, we specialize in genetics billing that optimizes reimbursements and minimizes denials. Our experienced coders stay current with evolving policies and payer requirements.




Genetics Billing Made Easy for Labs and Counselors
At MedicalBiller.co, we specialize in genetic testing and counseling billing—covering hereditary cancer panels, prenatal diagnostics, pharmacogenomics, and rare disease assays. We understand complex test codes, payer edits, and clinical documentation requirements.
Whether you're a genetic counselor, diagnostic lab, or integrated clinic, our compliant workflows and payer expertise help you capture full value. We stay current with CMS, NGS modifiers, LDT policies, and commercial reimbursement rules.
What Sets Us Apart
- NGS, CPT‑based & LDT billing expertise
- Genetic counseling and telehealth support
- Payer policy tracking (Medicare, Medicaid, Commercial)
- Appeal handling for medical necessity denials
- Lab & EHR integration via HL7/FHIR/API

Mission Statement
We streamline billing for genetics providers and labs—ensuring accurate coding, timely reimbursement, and full policy compliance. Your focus remains on patient outcomes, while we handle the financial details.
Why Choose MedicalBiller.co for Genetics Billing
Genetics billing involves nuanced coding (NGS, modifier reporting, multiple panels), evolving payer rules, and clinical documentation requirements. We help you reduce denials, accelerate pay, and simplify billing for advanced testing and counseling.
Watch the VideoNGS & Rare Disease Coding
Accurate CPT, HCPCS, and LOINC coding for panels, single-gene tests, and whole exome/profiles.
Compliance & Modifier Precision
Using gene-specific modifiers and clinical support documentation to meet payer policies.
Rapid Submission Turnaround
Claims submitted within 24 hours of final report delivery to reduce delays and denials.
Data-Driven Reporting
Dashboard insights on payer approvals, denial reasons, test volume, revenue per gene/test type.
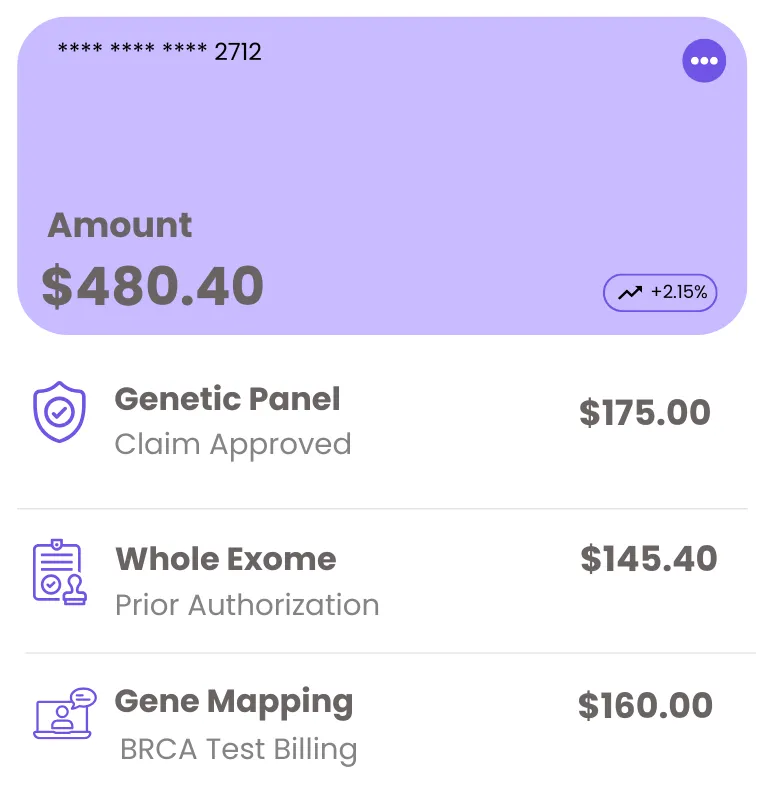
Transparent Genetics Billing Plans
Whether you're a small lab or a large genetic counseling practice, we provide scalable pricing based on test volume and complexity. No hidden fees, no confusion—just results-driven billing.
What’s Included
- Full service NGS, panel, single-gene billing
- Genetic counseling & telehealth billing
- Denial prevention & appeal submission
- Comprehensive reporting & payer analytics
Custom plans available based on complexity and integration needs.
Genetic Billing Workflow Built for Accuracy & Speed
Our process is designed to support genetic labs and practices with accurate coding, seamless data flow, payer compliance, and faster reimbursements—from test ordering and lab reporting to claim submission and denial management.

Test Review & Strategy
We evaluate your lab tests, panels, CPT/PLA codes, and workflow to build a payer-compliant billing plan.

EMR & Lab Integration
We integrate with your EMR or LIMS, import reports, and begin payer credentialing or authorizations if needed.

Coding & Claim Filing
We assign accurate CPT/PLA codes, attach documentation, and file claims within 24 hours of test completion.
Follow-Up & Reporting
We monitor payment status, resolve denials, and provide payer-specific analytics by test, code, and client.
0%
Genetic Test Claim Accuracy
0 Days
Avg. Reimbursement Time
0%
Avg. Revenue Increase
Genetic Billing Solutions for Precision & Compliance
We specialize in billing for genetic testing labs and counseling services—covering hereditary panels, single-gene tests, exome sequencing, and more. Our experts manage coding, submission, and denials while keeping up with fast-changing payer policies.
NGS & Molecular Coding
Accurate CPT/HCPCS coding for single-gene, panel, and whole exome sequencing with payer-specific guidelines.
Modifier & Medical Necessity Audits
Ensure compliant use of modifiers (e.g., 59, TC/26) and documentation that supports medical necessity for tests billed.
24-Hour Claim Submission
All claims submitted within 24 hours of final report, reducing delays and improving first-pass approval rates.
Appeals & Denial Management
We appeal denied claims with complete lab documentation and clinical support to maximize reimbursements.
Patient Statement & Support
Clear communication with patients regarding balances, EOBs, and insurance coverage on genetic services.
Test & Payer Performance Reporting
Detailed insights into reimbursement by payer, denial reasons by test, and revenue forecasts by test type.
What Our Clients Are Saying
Trusted by healthcare providers, billing managers, and business owners nationwide.
“ The team at MedicalBiller.co has made our billing operations smoother than ever. Their support is top-notch, and their response time is fantastic. ”
“ Their website made it incredibly easy to find the right billing service provider for our specialty. Everything is well-organized and tailored for healthcare needs. ”
“ I highly recommend MedicalBiller.co for any medical practice looking to outsource billing. They understand both the technical and human side of revenue cycle. ”
“ We've worked with several billing companies in the past, but MedicalBiller.co stands out with their accuracy, transparency, and proactive communication. ”
“ Their claim turnaround time is impressive, and we’ve seen a significant drop in denials since we partnered with MedicalBiller.co. ”
“ From credentialing to collections, they handle everything with professionalism. It's like having an in-house billing department without the overhead. ”
Frequently Asked Questions
Questions about our genetics billing solutions, CPT/PLA code handling, denials, EMR/LIMS integration, and payer compliance.
Speak with a Genetic Billing Expert
Whether you're a genetic testing lab, molecular diagnostics facility, or specialty clinic, we’re here to simplify your billing. Reach out for a free consultation on coding, compliance, and faster reimbursements.
IL 62701 United States






