Oncology Billing That Supports Complex Cancer Care
From chemotherapy infusions and radiation treatments to genetic testing and cancer staging, our oncology billing experts ensure accurate charge capture, prior authorizations, and timely reimbursement. We help oncology practices reduce denials, improve cash flow, and stay compliant with payer-specific rules and NCCI edits.




Oncology Billing Services Built for Precision and Compliance
At MedicalBiller.co, we provide specialized billing solutions for oncology practices, cancer centers, and infusion clinics. Our team understands the intricacies of oncology coding—from chemotherapy drugs and radiation oncology services to biopsies, lab tests, and pre-treatment authorizations.
We manage everything from J-code and CPT validation to CMS MUEs, modifier usage, and NCD/LCD compliance. Whether you provide medical, surgical, or radiation oncology, our billing workflows are designed to prevent denials, shorten payment cycles, and simplify audits.
What Sets Us Apart
- Chemotherapy & Infusion Coding (J-codes, 964xx)
- Radiation Oncology Billing & Global Period Management
- Pre-authorization & Eligibility Verification for High-Cost Drugs
- Denial Management for NCCI & LCD Edits
- Integration with ARIA, Mosaiq, Epic, and eClinicalWorks

Mission Statement
We help oncology providers focus on saving lives—while we take care of revenue, compliance, and clean claim processing. Our mission is to support cancer care delivery with accurate billing that reflects clinical complexity and payer expectations.
Why Oncologists Choose MedicalBiller.co
Oncology billing involves complex drug administration codes, prior authorizations, bundled payments, and strict documentation protocols. Our oncology billing team is fluent in J-codes, 96413/96417 infusions, and payer-specific rules—ensuring your revenue is protected while your focus stays on patient care.
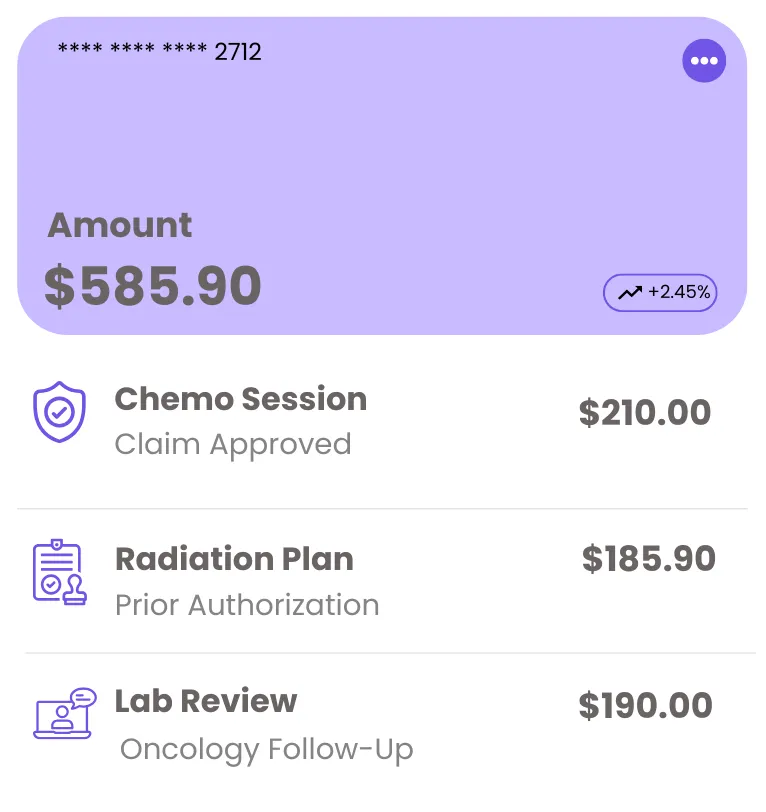
Infusion & Chemotherapy Billing
We manage timed infusions, hydration services, and drug administration using accurate CPT & HCPCS codes.
Pre-Auth & Payer Compliance
Our team handles prior auths for high-cost oncology drugs and tracks payer-specific documentation requirements.
Oncology Revenue Experts
Specialized account managers experienced in oncology coding, NCCI edits, MUEs, and clean claim strategies.
100% HIPAA-Compliant
We secure PHI with the latest encryption standards and offer full audit trail support for OIG and payer reviews.
Flexible Oncology Billing Packages
We offer performance-based pricing tailored to your oncology practice. Whether you’re running a standalone infusion center or a multi-specialty cancer clinic, our plans are built to scale—no hidden fees, no long-term contracts.
Cancer Centers & Multi-Physician Groups
Built for high-volume oncology practices billing $30,000+/month.
What’s Included
- Chemotherapy, immunotherapy, & infusion billing
- Authorization & eligibility verification
- Appeals & denial resolution for oncology claims
- Monthly analytics & revenue performance reports
Need custom pricing for a regional cancer network? Let’s explore a solution tailored to your operations.
Oncology Billing Made Simple in 4 Strategic Steps
From high-cost infusion drugs to bundled chemotherapy sessions, our oncology billing process is built for accuracy, compliance, and maximum reimbursement—backed by specialists who understand payer edits and NCCI rules.

Practice Audit & Payer Review
We evaluate your EMR setup, infusion workflow, fee schedule, and payer mix to design a billing strategy specific to oncology.

System Integration & Onboarding
We integrate with your EHR (e.g., Aria, Epic, eClinicalWorks), confirm billing credentials, and map your service codes and modifiers.

Charge Capture & Coding
We validate all CPT, ICD-10, and HCPCS codes for chemotherapy, infusions, and E&M services—ensuring claim accuracy before submission.
Claim Follow-Up & Insights
We track every claim, handle denials or audits promptly, and deliver custom reports showing drug margins, payments, and payer trends.
0%
Oncology Claim Accuracy Rate
0 Days
Average Reimbursement Time
0%+
Average Revenue Growth for Oncology Groups
Oncology Billing Services That Safeguard Your Revenue
From chemotherapy and radiation billing to infusion coding and drug authorization, our oncology billing team ensures precise claim handling and faster collections—so your practice remains financially strong and fully compliant.
Chemotherapy & Infusion Billing
Accurate billing for 96413/96417, hydration therapy, and injection services with proper start/stop time tracking.
J-Code Drug Management
We ensure clean usage of high-cost injectable drug codes (e.g., J9355, J9190) with linked diagnoses and prior auth documentation.
24-Hour Charge Entry
All charges for infusions, consults, and labs are processed within one business day to prevent delays in revenue cycle.
Denial Defense & Resubmissions
We resolve rejected oncology claims due to bundling conflicts, missing modifiers, or unsupported codes—fast and thoroughly.
Patient Benefits & Cost Guidance
We verify oncology coverage and help patients understand co-pays, drug copay assistance, and financial eligibility options.
Oncology Revenue Dashboards
We provide real-time reports on drug utilization, payment velocity, payer trends, and service-specific revenue insights.
What Our Clients Are Saying
Trusted by healthcare providers, billing managers, and business owners nationwide.
“ The team at MedicalBiller.co has made our billing operations smoother than ever. Their support is top-notch, and their response time is fantastic. ”
“ Their website made it incredibly easy to find the right billing service provider for our specialty. Everything is well-organized and tailored for healthcare needs. ”
“ I highly recommend MedicalBiller.co for any medical practice looking to outsource billing. They understand both the technical and human side of revenue cycle. ”
“ We've worked with several billing companies in the past, but MedicalBiller.co stands out with their accuracy, transparency, and proactive communication. ”
“ Their claim turnaround time is impressive, and we’ve seen a significant drop in denials since we partnered with MedicalBiller.co. ”
“ From credentialing to collections, they handle everything with professionalism. It's like having an in-house billing department without the overhead. ”
Frequently Asked Questions
Answers to common questions about our oncology billing expertise, chemotherapy coding, drug reimbursements, and compliance strategies.
Get in Touch with Our Oncology Billing Experts
Whether you operate an independent cancer clinic or a hospital oncology department, our billing experts are ready to optimize your revenue. Let’s talk about reducing denials, accelerating reimbursements, and ensuring full compliance with complex oncology billing protocols.
IL 62701 United States






