Reclaim Lost Revenue with Urology-Specific Billing Precision
Urology billing involves intricate combinations of E/M visits, in-office procedures, diagnostics, and global surgical packages. We streamline these complexities to help your practice avoid denials, optimize reimbursements, and stay compliant with payer policies.



Comprehensive Billing Built Around Urological Care
Urology billing requires deep knowledge of surgical bundles, diagnostic testing, office-based procedures, and frequent use of modifiers. Our team is trained to handle the nuanced coding of cystoscopies, biopsies, BPH treatments, and more—with special attention to payer-specific rules.
We don't just code claims; we improve revenue strategy. Our team works alongside your clinical and admin staff to track payment trends, spot underpayments, and implement real-time fixes—all while maintaining full HIPAA compliance and billing transparency.
Why Urology Practices Choose Us
- Global Surgical Package Tracking & Post-Op Billing Support
- Clean Coding for Cystoscopies, Urodynamics, & In-Office Procedures
- Modifiers Managed for Bilateral, Repeat, or Assistant Services
- Automated Eligibility Checks for Medicare, Medicaid & Commercial Plans
- Timely Filing & Denial Appeals to Maximize Collections

Our Mission
To reduce administrative stress for urology teams by simplifying billing, securing full reimbursements, and providing accurate financial visibility—so providers can focus entirely on patient outcomes.
Why Urology Practices Count on Our Billing
Urology billing involves unique combinations of office visits, diagnostic tests, and surgical codes—all requiring careful modifier use and proper bundling. Our systems are calibrated to catch costly errors before claims go out.
Modifier Accuracy
Our coders ensure correct use of modifiers—especially 25, 51, 59, and 76—reducing denials on bundled and global services.
Global Period Tracking
We manage global surgical periods across all urologic procedures to avoid billing violations and duplication.
Procedure-to-Diagnosis Mapping
We link each CPT code to medically necessary ICD-10s that pass payer edits and medical necessity rules.
Surgical & In-Office Coverage
From TURPs to vasectomies to BPH injections, we bill all urological procedures correctly—regardless of setting.
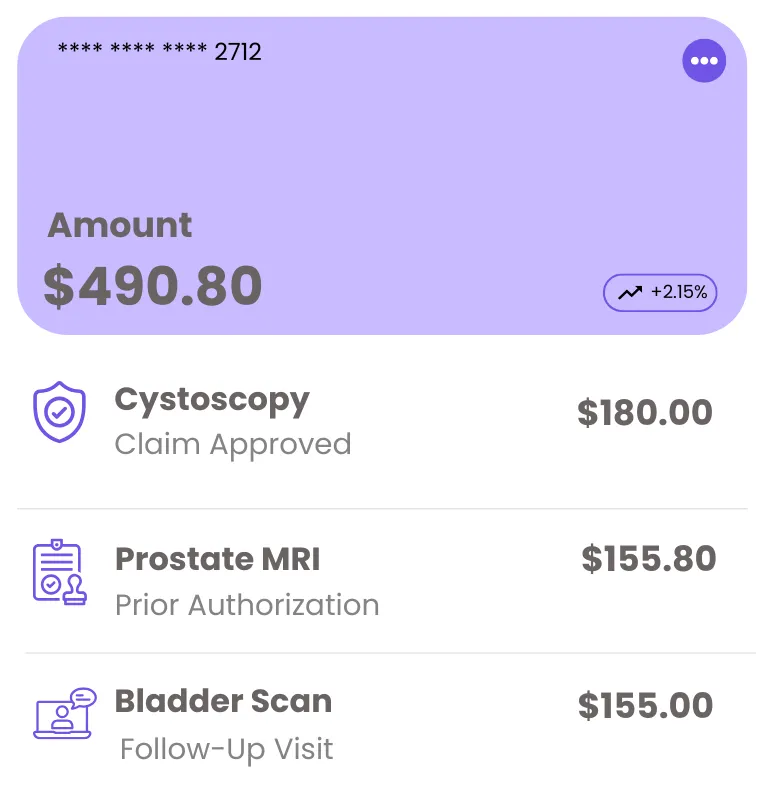
Simple Pricing. No Surprises.
Our urology billing rates are built around your practice size and service mix. From solo urologists to surgical groups, we customize billing fees based on what you actually need.
Private Practice
1–2 providers focused on outpatient care
Surgical Urology Groups
For practices with 3+ providers and surgical billing volume
Included Services
- Daily coding, charge entry, and batching
- Modifier validation and bundling compliance
- Procedure-specific payment tracking
- Monthly reports on denials, trends, and payers
Running multiple locations? We’ll tailor billing workflows per site.
A Seamless Billing Process for Urology
Our billing process adapts to your EHR, surgery schedule, and practice style—keeping the work behind the scenes clean and consistent.

Practice Review
We analyze your services, coding habits, and payer patterns to design the right billing framework.

System Integration
We connect with your PM/EHR system to enable smoother charge capture and eligibility verification.

Billing in Motion
We handle claims daily, review rejections immediately, and stay ahead of payer policy updates.
Feedback & Forecasting
We provide monthly analysis, highlight improvement areas, and help you forecast revenue trends accurately.
0%
Procedure Coding Accuracy on First Pass
0 Days
Median Days from Claim to Payment
0%
Revenue Growth in First 90 Days
Comprehensive Billing for Urology Practices
From office-based procedures to hospital surgeries, our billing support adapts to the full scope of your urology services. We navigate coding rules, payer variations, and authorization requirements—so you don’t have to.
Procedure & Surgery Coding
From cystoscopies to vasectomies and urodynamic studies, we code everything with full documentation review and modifier use where needed.
Pre-Authorizations & Benefits Checks
We obtain prior auth for procedures and confirm benefits before scheduling, preventing costly denials or last-minute cancellations.
Claim Submission & Follow-Up
Claims are reviewed, scrubbed, and submitted within 24 hours—then tracked daily for denials, underpayments, and missed remits.
Patient Statements & Phone Support
Our bilingual billing support team helps patients understand balances, coverage, and payment options—without tying up your front desk.
Performance Reporting
We break down revenue by provider, procedure, and location—so you can see which services drive results and where improvements are needed.
Appeals & Coding Compliance
We don’t just resubmit denials—we identify root causes, write effective appeals, and make sure documentation supports billing accuracy.
What Our Clients Are Saying
Trusted by healthcare providers, billing managers, and business owners nationwide.
“ The team at MedicalBiller.co has made our billing operations smoother than ever. Their support is top-notch, and their response time is fantastic. ”
“ Their website made it incredibly easy to find the right billing service provider for our specialty. Everything is well-organized and tailored for healthcare needs. ”
“ I highly recommend MedicalBiller.co for any medical practice looking to outsource billing. They understand both the technical and human side of revenue cycle. ”
“ We've worked with several billing companies in the past, but MedicalBiller.co stands out with their accuracy, transparency, and proactive communication. ”
“ Their claim turnaround time is impressive, and we’ve seen a significant drop in denials since we partnered with MedicalBiller.co. ”
“ From credentialing to collections, they handle everything with professionalism. It's like having an in-house billing department without the overhead. ”
Urology Billing—Answers to What Urologists Ask Most
Billing for urology involves surgical coding, diagnostic testing, and payer-specific nuances. We’ve compiled answers to the questions we frequently receive from urology clinics and providers.
Streamline Urology Billing with Confidence
Whether you're managing multiple office locations or expanding surgical services, our team is ready to simplify your urology billing. Let’s discuss how we can support your practice with reliable, specialty-focused RCM solutions.
Atlanta, GA 30339






