In clinical practice, documentation and coding are more than administrative necessities—they directly impact patient care, reimbursement, and compliance. While the day-to-day clinical duties focus on diagnosis and treatment, accurate coding ensures those efforts are appropriately represented and compensated.
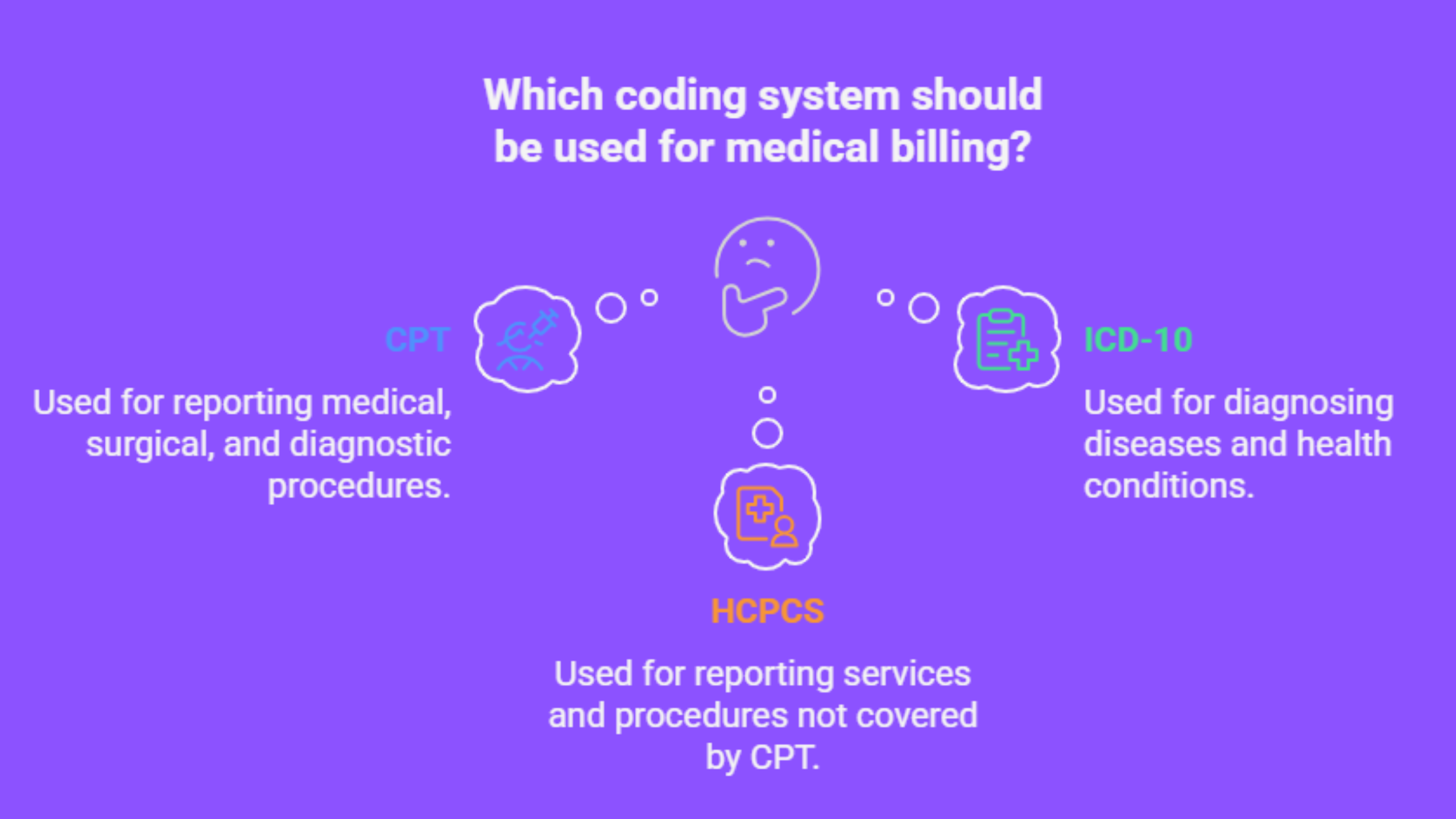
Three primary medical coding systems—CPT, ICD-10, and HCPCS—play distinct but interconnected roles in this process. If you’ve ever wondered exactly how they differ, and when each should be used, this article offers a clear and concise breakdown.
CPT, ICD-10, and HCPCS at a Glance
| Code Set | Full Name | Purpose | Maintained By |
|---|---|---|---|
| CPT | Current Procedural Terminology | Describes medical, surgical, and diagnostic services | American Medical Association (AMA) |
| ICD-10 | International Classification of Diseases, 10th Revision | Classifies diseases and health conditions | World Health Organization (WHO); U.S. version by CDC |
| HCPCS | Healthcare Common Procedure Coding System | Covers services, supplies, and equipment not in CPT | Centers for Medicare & Medicaid Services (CMS) |
Each system has a unique purpose, but they frequently work together on claims and documentation. Let’s explore them in detail.
What is CPT?
Current Procedural Terminology (CPT) codes are used to describe what was done during a patient visit—procedures, treatments, surgeries, diagnostic services, and more.
Developed and maintained by the American Medical Association (AMA), CPT codes are widely used in outpatient and office settings across the United States.
Key Characteristics of CPT Codes
-
Format: 5-digit numeric codes (e.g.,
99213,93000) -
Categories:
-
Category I: Standard codes for commonly performed procedures (e.g., office visits, lab tests)
-
Category II: Optional performance measurement codes
-
Category III: Temporary codes for emerging technology and services
-
-
Updated Annually: CPT codes are revised every year to reflect new procedures and retire outdated ones.
When CPT Is Used
CPT codes appear on most outpatient claims to report services such as:
-
Office and hospital visits
-
Minor and major surgeries
-
Imaging (X-rays, MRI, CT)
-
Laboratory services
-
Preventive care
For example, if a physician performs a Level 3 established patient visit, they’ll use 99213 as the CPT code.
What is ICD-10?
International Classification of Diseases, 10th Revision (ICD-10) codes describe why a patient is receiving care—namely, the diagnosis, symptom, or condition being evaluated or treated.
In the U.S., ICD-10 is used in the form of ICD-10-CM (Clinical Modification). It’s maintained by the Centers for Disease Control and Prevention (CDC) in collaboration with the World Health Organization (WHO).
Key Characteristics of ICD-10-CM Codes
-
Format: Alphanumeric codes starting with a letter followed by up to six digits (e.g.,
E11.9for Type 2 diabetes without complications) -
Granular Detail: ICD-10 offers specificity for laterality (left/right), episode of care, and complication status.
-
Purpose:
-
Medical necessity documentation
-
Disease tracking
-
Epidemiological research
-
Reimbursement justification
-
When ICD-10 Is Used
ICD-10 codes are required for both outpatient and inpatient claims. Every service billed must be linked to at least one diagnosis code to justify its medical necessity.
For example, a patient receiving care for uncontrolled hypertension may be assigned I10, which denotes essential (primary) hypertension.
What is HCPCS?
Healthcare Common Procedure Coding System (HCPCS) expands upon CPT codes and is primarily used for Medicare and Medicaid billing. It includes items not found in the CPT code set, such as medical equipment, ambulance services, and certain medications.
Developed and managed by the Centers for Medicare & Medicaid Services (CMS), HCPCS consists of two levels:
Level I: CPT Codes
-
Essentially the AMA CPT code set
-
Used universally in billing for procedures and services
Level II: HCPCS Codes
-
Alphanumeric codes (1 letter + 4 digits), e.g.,
E0110for a standard crutch -
Covers products, supplies, and services not included in CPT
-
Durable medical equipment (DME)
-
Prosthetics and orthotics
-
Ambulance services
-
Injectable drugs
-
Some dental procedures
-
When HCPCS is Used
While commercial insurers may occasionally require HCPCS Level II codes, they are essential for:
-
Medicare and Medicaid claims
-
Reporting non-physician services and products
-
Billing for supplies used in outpatient care
For instance, if a patient is issued a wheelchair, the provider would use E1234 (example code) to report it.
Summary of Key Differences
| Feature | CPT | ICD-10 | HCPCS |
|---|---|---|---|
| Describes | Procedures and services | Diagnoses and conditions | Supplies, drugs, services |
| Format | 5-digit numeric (e.g., 99214) | Alphanumeric (e.g., J45.909) | Alphanumeric (e.g., A0428) |
| Used For | What was done | Why it was done | What else was needed |
| Managed By | AMA | CDC/WHO | CMS |
| Primary Use | Reimbursement & documentation | Diagnosis justification | Medicare billing & non-CPT items |
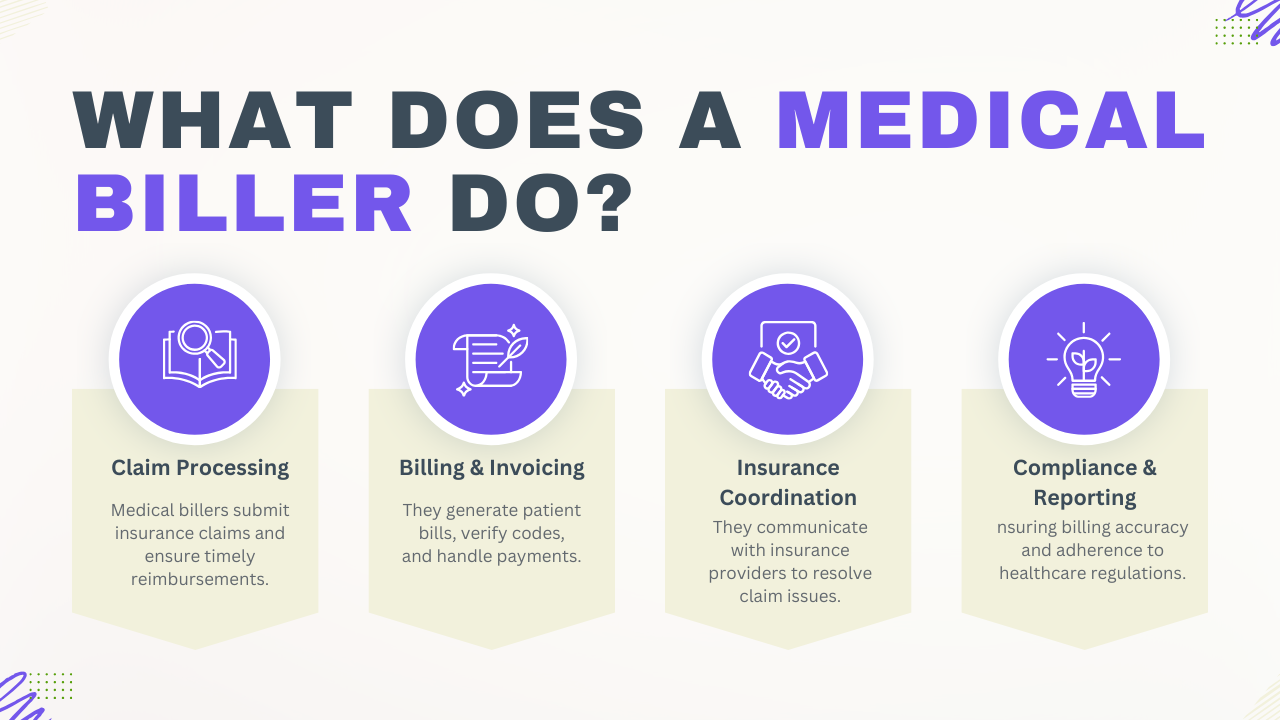
How They Work Together
In clinical documentation and billing, these code sets are used in concert:
-
ICD-10 explains the patient’s condition (e.g.,
I25.10– CAD without angina) -
CPT describes the treatment (e.g.,
92928– coronary stent placement) -
HCPCS may supplement with supplies or services (e.g.,
A4649– surgical supply)
A proper claim must establish that the procedure (CPT or HCPCS) was medically necessary (supported by ICD-10).
Incorrect or mismatched codes often lead to denied claims or audit risk, emphasizing the importance of coding accuracy and compliance.
Common Pitfalls and Best Practices
-
Overlooking Specificity in ICD-10
Choose the most detailed code available. Using vague codes like “unspecified” can flag claims for review. -
Using CPT When HCPCS Is Required
For Medicare claims, confirm whether the service or item is listed under HCPCS Level II. -
Assuming One Code Set Covers All
Every visit requires a diagnosis (ICD-10) and a procedure (CPT or HCPCS)—not one or the other. -
Not Keeping Up with Updates
All three systems are updated annually. Outdated codes are a common cause of claim denials.
Final Thoughts
For providers, CPT, ICD-10, and HCPCS may feel like layers of red tape. But when used correctly, they are a structured language that allows the healthcare system to function—ensuring that care is understood, justified, and reimbursed.
Understanding the distinctions between them doesn’t require a coding certification—but having a clear grasp of each code set's role is essential for reducing errors, improving compliance, and safeguarding revenue.
If you're a physician or healthcare administrator looking to improve documentation and reduce denials, focusing on these three code sets is a critical first step.