A Straightforward Explanation for Healthcare Providers
The Advance Beneficiary Notice of Noncoverage (ABN) is a critical document used in Medicare billing. It's not just another form to file away—it's a safeguard for both providers and patients. Issued before delivering services or items that Medicare is likely to deny, the ABN serves to notify patients that they may be financially responsible for certain care if it’s not covered.
Understanding how and when to use an ABN helps ensure compliance, reduce claim denials, and maintain transparency with patients. If your practice serves Medicare beneficiaries, the ABN is something your front desk staff, billing department, and clinical team must all be familiar with.
What Exactly Is an ABN?
An ABN (CMS Form R-131) is a written notice a provider gives to a Medicare beneficiary when Medicare may not pay for a particular service or item. It gives the patient the opportunity to make an informed decision about whether to proceed and accept financial responsibility if coverage is denied.
The ABN isn't optional in these situations—it's a legal requirement under Medicare regulations. Without it, providers cannot bill the patient if the service is later denied, even if the denial was fully anticipated.
When Do You Need to Use an ABN?
The ABN is required when:
-
A service is not considered medically necessary based on Medicare's Local Coverage Determination (LCD) or National Coverage Determination (NCD) guidelines.
-
Frequency limits have been exceeded (e.g., a lab test already performed within the covered timeframe).
-
Services are preventive or routine and not covered under the patient’s Medicare plan (e.g., regular eye exams or physicals).
-
The patient requests a non-covered item or service, such as cosmetic procedures or certain convenience DME upgrades.
If there's any reason to believe Medicare will deny coverage, the ABN should be issued before the service is rendered—not after. The timing is important: delivering the form retroactively makes it invalid, and billing the patient in those cases can result in non-compliance penalties or financial liability falling back on your practice.
What's Included in an ABN?
An ABN contains several essential elements:
-
Patient Information – Name and identification
-
Description of Service – Clearly identifies the item or service in question
-
Reason Medicare May Not Pay – Explains why the item may be denied (e.g., “Medicare does not cover this service more than once every 12 months”)
-
Estimated Cost – A reasonable cost estimate for the patient
-
Patient Options – The patient must choose whether to:
-
Receive the service and accept responsibility if denied
-
Refuse the service
-
-
Signature and Date – To document acknowledgment
The language must be clear and specific. Vague or overly technical explanations can invalidate the form. Medicare wants patients to truly understand what they're signing—not feel forced or confused.
Why the ABN Matters
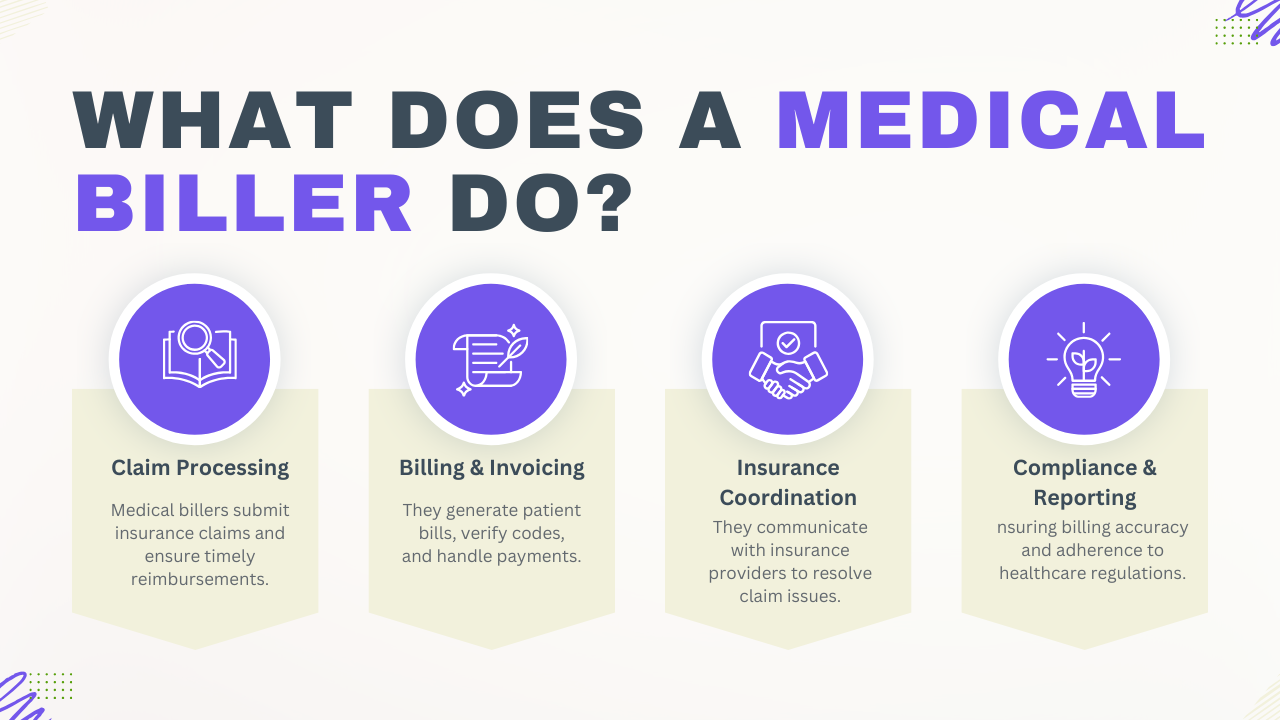
For providers, the ABN serves three main purposes:
1. Protecting Reimbursement Rights
If Medicare denies a claim and no valid ABN was given in advance, the provider cannot charge the patient. The loss becomes the provider's responsibility.
2. Avoiding Legal and Compliance Issues
Failure to issue ABNs appropriately can lead to audits, penalties, or allegations of improper billing. Inconsistent or incorrect use may even trigger reviews by CMS or Medicare Administrative Contractors (MACs).
3. Patient Transparency and Trust
Patients deserve to know if they might be on the hook for a bill. The ABN provides clarity up front. It also improves patient relationships when handled with professionalism and empathy.
Common Scenarios That Require an ABN
To better understand practical application, here are a few examples where an ABN should be issued:
-
A patient comes in for a screening colonoscopy, but has already received one within 10 years. Medicare may not cover a second procedure without a qualifying reason.
-
A patient requests a custom foot orthotic, which is not covered unless there’s a qualifying diagnosis that meets strict medical necessity.
-
A lab test is being ordered that exceeds the frequency limit set by Medicare guidelines.
-
A patient opts for a preventive physical exam, which Medicare doesn’t typically cover in the way commercial insurers do.
In all these cases, providing an ABN is not about discouraging the patient from care—it’s about ensuring they understand their options and the possible financial responsibility.
Who Can Issue an ABN?
An ABN can be issued by:
-
Physicians and non-physician practitioners
-
Hospitals
-
Labs
-
Durable Medical Equipment (DME) suppliers
-
Home health and hospice agencies
-
Outpatient therapy providers
In short, any Medicare-enrolled provider or supplier offering services that may be denied by Medicare must use the ABN appropriately.
Note: ABNs are not used in emergencies or for services that are statutorily excluded from Medicare, such as hearing aids or most dental services. In those cases, other notice types (such as a voluntary notice) may apply.
Proper ABN Workflow in a Clinical Setting
Implementing a reliable ABN workflow helps avoid errors. Here’s how a streamlined process might look:
-
Service Ordered
The provider recommends a test, treatment, or item. -
Eligibility/Medical Necessity Check
Billing staff or EHR software reviews coverage policies (LCDs/NCDs). -
Coverage Question Identified
If medical necessity is questionable or frequency exceeded, an ABN is triggered. -
ABN Completion and Discussion
Staff completes the ABN, explains it to the patient in understandable terms, and answers any questions. -
Patient Decision and Signature
The patient selects an option, signs, and receives a copy. -
Service Rendered
Provider delivers the service, and billing proceeds based on outcome.
Common ABN Mistakes to Avoid
Even experienced billing staff can occasionally get it wrong. Here are some of the most frequent errors:
-
Failing to issue an ABN before the service is rendered
-
Using outdated ABN forms (Always use the latest CMS-approved version)
-
Leaving out estimated costs
-
Pre-checking option boxes (Patients must select their choice)
-
Poor explanations of non-coverage reasons
-
Getting signatures under pressure or without time to review
Avoiding these mistakes helps ensure your ABNs are legally valid and ethically sound.
How Long Should ABNs Be Kept?
Per CMS guidelines, providers should retain a copy of the signed ABN for at least 5 years from the date of care or the completion of billing—whichever is later. For services related to cost reports (such as for hospital providers), a longer retention period may be required.
Read complete guidelines here:
https://www.cms.gov/files/document/mln006266-medicare-advance-written-notices-non-coverage.pdf
Final Thoughts
The Advance Beneficiary Notice is not just a form—it’s a key part of delivering Medicare-compliant care. Used properly, it supports informed patient decisions, strengthens billing integrity, and protects your practice from unnecessary write-offs.
Every team member involved in patient interaction or billing should be trained on ABN protocols. It’s not just the billing department’s responsibility; front-desk staff, clinical assistants, and providers must all understand the basics of when and how to use it.
In a landscape where regulatory scrutiny and patient financial concerns continue to grow, the ABN helps keep communication clear, decisions informed, and compliance intact.
Quick Summary:
-
ABN = Advance Beneficiary Notice of Noncoverage
-
Used when Medicare may deny a service/item
-
Must be issued before the service is provided
-
Protects the provider’s right to bill the patient
-
Must be clear, specific, and signed
-
Errors can lead to compliance risks or denied payments
Understanding the ABN process is not just about getting reimbursed—it's about delivering responsible care with transparency and professionalism.